Pharmaceutical Sciences. 2025;31(3):313-321.
doi: 10.34172/PS.025.40700
Research Article
Comparison of Deep Neuromuscular Block in Inhalation and Total Intravenous Anesthesia on Peritoneal Compliance and Surgical Conditions During Laparoscopic Cholecystectomy
Maryam Khoubnasabjafari Conceptualization, Formal analysis, Methodology, Writing – review & editing, 1, 2 
Mahmood Eidi Formal analysis, Investigation, 2
Hamzeh Hosseinzadeh Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing, 2, * 
Author information:
1Tuberculosis and Lung Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Anesthesiology and Intensive Care, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Background:
Deep relaxation leads to improved surgical outcomes by providing more successful surgical conditions. In this study, the effect of rocuronium-induced deep relaxation on abdominal compliance and surgeon satisfaction in total intravenous anesthesia (TIVA) and inhalation anesthesia (IA) methods is investigated. The xiphopubic distance (XPD) is proposed as a simple measure of abdominal laxity.
Methods:
After premedication, 70 candidate patients for laparoscopic cholecystectomy (LC) are divided to TIVA and IA groups. In TIVA, propofol infusion at a dose of 60-100 μg/kg/min, and in IA isoflurane with MAC of 1-2 were used. After stabilization of intra-abdominal pressure (IAP), rocuronium is injected at a dose of 0.3 mg/kg to provide train of four (TOF)=0 and post tetanic count (PTC)=0. To check the degree of abdominal wall relaxation, the XPD is measured at 3 stages. The level of satisfaction of the surgeon is recorded. At the end of surgery, when TOF receiving at least two responses, the anesthetic drugs are discontinued and antagonized.
Results:
The mean and frequency of most of the studied variables were the same in TIVA and IA groups and the observed differences were not statistically significant. The average change of heart rates in TIVA was significantly more than IA, and the arterial oxygen saturation in IA was more than TIVA. Deep relaxation and IAP of 15 mm Hg provided better surgical conditions, peritoneal compliance and surgeon’s satisfaction in both TIVA and IA methods and recovery was associated with the acceptable postoperative outcomes. The employed procedure does not require sugammadex as a reversing agent which reduces the cost of surgery.
Conclusion:
The deep relaxation induced by rocuronium in LC along with favorable IAP, good vision on the field and suitable surgical conditions in both IA and TIVA methods, and the difference in the findings related to the methods were not significant. Considering all aspects, the use of deep relaxation is recommended in LC with both anesthesia methods.
Keywords: Deep relaxation, Inhalation anesthesia, Intravenous anesthesia, Rocuronium, Laparoscopic cholecystectomy, Xiphopubic distance
Copyright and License Information
© 2025 The Author(s).
This is an open access article and applies the Creative Commons Attribution Non-Commercial License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
This work is partially supported by Tabriz University of Medical Sciences under the project number of 68782.
Introduction
Gallstones are the most common cause of recurrent abdominal pain, which is often accompanied by nausea and vomiting. The frequency of gallstones increases with age, in women and in obese people, and most of them are asymptomatic. Gallstone disease is the most common reason for patients with abdominal symptoms to visit the hospital. Complications caused by gallstones include chronic inflammation, cholecystitis, abscess formation, and obstruction of the bile ducts, which lead to jaundice, severe ascending infection, and pancreatitis which effectively treated with cholecystectomy surgery. The rate of total cholecystectomy (both laparotomy and laparoscopy) was 62-213 per 100 000 in European countries in year 2003.1 The golden treatment for gallstones is laparoscopic cholecystectomy (LC) with advantages of shorter hospitalization, smaller incisions, faster return to normal function, and fewer side effects.2
Operation conditions in LC are important factors in the success rate of surgery and are controlled by factors either related or non-related to the patient. Obesity, previous pregnancies, and history of abdominal surgeries are factors related to the patient, and the type of anesthesia, the amount of intra-abdominal pressure (IAP), and the position of the patient during surgery are not-related factors to the patient.3 LC benefits from deep relaxation since small movement of the patient may cause significant effects in surgical conditions. A surgeon who has to work in a closed space with limited visibility and to facilitate surgery, they use carbon dioxide insufflation, but at the same time, it should be kept in mind that IAP causes many pathophysiological changes in the cardiovascular and respiratory systems. After insufflation the gas in the abdominal cavity, systemic resistance and pulmonary vascular resistance increase and cardiac output decreases by 1%-30%.4 The increase in IAP caused by insufflation more gas and with high pressure causes more changes in hemodynamics, and in the meantime CO2 absorption increases and exerts more physiological effects on the cardiovascular, pulmonary and renal systems. Any factor such as anesthesia or deep muscle relaxation that reduces IAP and reduces CO2 absorption will decrease hemodynamic changes in LC.5 The level of neuromuscular block and IAP are important factors in the success of laparoscopic procedure and managing the postoperative complications.6 Deep relaxation effects with rocuronium increase the compliance of the abdominal cavity and improve the field of vision at the same pressure. On the other hand, the use of deep relaxation has problems in the recovery of the patients, and the available evidence shows that the relaxation remains up to 50%, even after the use of muscle relaxants with moderate effect and the use of anticholinesterases to reverse the relaxation. With the introduction of sugammadex, there is a possibility of rapid reverse of relaxation, even after deep relaxation7 and if sugammadex is available, there is no reason to avoid using deep relaxation. It should be noted that the benefits of maintaining a deep muscle block during surgery have not been fully studied.8 Results of further studies show that the costs of using high doses of sugammadex are significant and may be an obstacle to the use of deep relaxation, especially in low-income communities.9
Total intravenous anesthesia (TIVA) and inhalation anesthesia (IA) are the most common methods of general anesthesia, and the selection of each of these methods is based on the experience of the anesthesiologist.10 The total number of side effects observed in TIVA was higher than that of IA, and the length of stay in the ICU was longer for IA (1.23 vs. 0.87 days). The results of investigations on intraperitoneal shunt and oxygenation in chest surgeries indicated the superiority of TIVA. In terms of hemodynamic parameters and cardiovascular complications, the situation has been in favor of IA.11
Neuromuscular blocking agents (NMBs) provide many advantages such as facilitated intubation and mechanical ventilation, maintained stable hemodynamics, longer surgery time without any reflex movements, and reducing the dose of anesthetic agents. Their metabolism is rapid and the metabolites are inactive and also could be used in renal and liver diseases.12 Among these drugs, rocuronium is an intermediate acting with the maximum blockade in 1-2 minutes, with 33% renal excretion and < 75 % hepatic elimination.13
In this study, the effect of deep block in LC will be studied in TIVA and IA groups. The reason for using a intermediate-acting NMB agent (rocuronium) is the relatively quick reverse of the deep neuromuscular blockade to the moderate block at the end of the surgery, which provides the possibility of reversing with neostigmine, and with this, it avoids the high cost of reversing the deep relaxation with sugammadex. In addition, the effects of deep neuromuscular block in two anesthesia methods (TIVA and IA) on surgical conditions and abdominal compliance were studies by surgeon’s scaling and measuring the xiphopubic distance (XPD) as a proposed measure of abdominal laxity. XPD is proposed as a simple quantitative measure for the extent of neuromuscular block in this work.
Materials and Methods
Participants
Seventy patients who are candidates for LC surgery after obtaining informed consent and meeting the inclusion criteria were enrolled in this study.
Randomization and blinding
The patients enrollment in this study is non-random, and after premedication they are randomly assigned to IA or TIVA group. The surgeon and the statistician are blinded on the details of the anesthesia procedure.
Anesthesia protocol
The patients are premedicated using midazolam (0.03 mg/kg) + fentanyl (1.5 µg/kg) injection. The electrodes of the neuromuscular stimulation device are placed in the path of the ulnar nerve to stimulate the adductor pollicis muscle. After premedication with fentanyl and midazolam, single twitches with the intensity of 20, 30, 40 and 50 are performed with Xavant Stimpod brand neurostimulator to obtain the basic response and the amount of supramaximal stimulation is calculated. Then they undergo induction with lidocaine (1.5 mg/kg) + propofol (1.5-2.5 mg/kg) + rocuronium (0.4 mg/kg). Muscle block is monitored every 15 seconds until train of four (TOF) = 0 (onset time), then intubation of patients is done and the patients are randomly divided into IA and TIVA groups. In IA group, isoflurane with MAC of 1-2, and in TIVA group, a continuous infusion of propofol (60-100 µg/kg/min) were administered. Infusion of remifentanil (0.05-0.1 µg/kg/min) along with a mixture of oxygen and air (in equal proportions) were used to maintain anesthesia in both groups. The data of all monitors are recorded every 3 minutes until insufflation gas in the peritoneal cavity. After insufflation CO2, stabilizing the IAP below 15 mm Hg and data collection, rocuronium is injected with a bolus dose of 0.3 mg/kg to obtain TOF = 0 and post tetanic count (PTC) = 0 (deep relaxation), and in this condition, the required data including IAP, hemodynamics and end-tidal CO2 are recorded. To check the degree of abdominal wall relaxation, the XPD (distance from xiphoid to symphysis pubis) was measured in three steps using a sterile ruler; i.e. before induction (D1), after gas insufflation (D2) and after deep relaxation following re-injection of rocuronium bolus dose and achieving TOF of zero (D3). The changes of XPD are calculated as
at different stages. The change in the flow of CO2 into the peritoneum, and the surgeon’s satisfaction with the surgical conditions are evaluated to increase the compliance of the abdomen and the comfort of the surgeon’s work. The surgeon reports satisfaction with the quality of the surgical conditions based on the five criteria.14 At the end of surgery, when TOF produces at least two responses, anesthetics are stopped and the muscle relaxation is reversed with the usual doses of neostigmine and atropine, and after achieving sufficient spontaneous breathing (negative inspiratory pressure > 20), the patients extubated and delivered to the recovery. The duration of TOF is recorded from 0 to 2, and in recovery, when TOF ratio is 0.9 and the Aldrete score is 10, the patient is discharged. Details of the study and allocation of the patients is illustrated as a flow chart in Figure 1.

Figure 1.
Flow chart of the study
.
Flow chart of the study
Sample size
Based on the sample size of similar studies, for example, 54 patients in the study of Turhanoğlu et al,15 70 patients who were candidates for elective LC surgery were included after obtaining the written consent.
Statistical methods
Collected data were analyzed using SPSS version 15.0. The differences among mean values in TIVA and IA groups were tested employing t-test. The χ2 analysis was used to test the differences in the frequencies and P < 0.05 was considered as a significant level.
Inclusion criteria
Patients who undergo LC surgery, aged 18-65 years, body mass index (BMI) less than 35, no allergy to the used drugs and have signed the informed consent form.
Exclusion criteria
No consent for contribution, BMI > 35, patients who are finally operated on and having any underlying diseases such as hypertension, short stature, having scars, having lung problems and the possibility of aspiration, liver and kidney problems, neuromuscular diseases and patients with current infection were the exclusion criteria.
Results and Discussion
Table 1 reports the mean and standard deviation (SD) of demographic and bio data of the patients. The differences observed are not statistically significant (P > 0.05). These findings indicate that the patients in TIVA and IA groups are matched which according to the random grouping method used in this study, were expected.
Table 1.
The mean and standard deviation of demographic and bio data of the patients in two groups
|
|
Total IV anesthesia
|
Inhalation anesthesia
|
P
value
|
|
Mean
|
SD
|
Mean
|
SD
|
| Age (y) |
45 |
12 |
46 |
10 |
0.61 |
| Weight (kg) |
76 |
11 |
79 |
11 |
0.33 |
| Height (cm) |
165 |
6 |
165 |
9 |
0.59 |
| BMI (kg/m2) |
28 |
4 |
29 |
4 |
0.16 |
| SBP (pre deep relaxation) (mm Hg) |
129 |
13 |
133 |
17 |
0.41 |
| DBP (pre deep relaxation) (mm Hg) |
79 |
10 |
84 |
12 |
0.05
|
| MAP (pre deep relaxation) |
96 |
10 |
100 |
12 |
0.09 |
| HR (pre deep relaxation) |
87 |
14 |
87 |
18 |
0.93 |
BMI, body mass index; SBP, systolic blood pressure; DBP, Diastolic blood pressure; MAP, Mean arterial pressure; HR, Heart rate.
Table 2 lists the mean and SD of the interoperative measured data of the patients and the P values for the t-test. The result of the t-test showed a significant (P = 0.02) difference between mean of SPO2 in TIVA (SPO2 = 96) and IA (SPO2 = 97) groups. This finding is not in agreement with the decreased PaO2 in IA group reported by others.16,17 However, two other works18,19 reported no significant change in pulmonary oxygen exchange.
Table 2.
The mean and standard deviation of the measured parameters of the patients in two groups
|
|
Total IV anesthesia
|
Inhalation anesthesia
|
P
value
|
|
Mean
|
SD
|
Mean
|
SD
|
| Rocuronium (mg) |
33.5 |
5.7 |
36.2 |
6.3 |
0.07 |
| SBP (post deep relaxation) (mm Hg) |
116 |
13 |
117 |
15 |
0.89 |
| SBP difference |
14 |
11 |
18 |
15 |
0.27 |
| DBP (post deep relaxation) (mm Hg) |
71 |
7 |
75 |
12 |
0.11 |
| DBP difference |
9 |
7 |
11 |
9 |
0.35 |
| MAP (post deep relaxation) |
86 |
8 |
89 |
11 |
0.23 |
| MAP difference |
10 |
7 |
12 |
10 |
0.32 |
| HR (post deep relaxation) |
75 |
11 |
80 |
15 |
0.10 |
| HR difference |
14 |
9 |
9 |
9 |
0.03
|
| SPO2 |
96 |
2 |
97 |
2 |
0.02
|
| ETCO2 |
31 |
4 |
31 |
2 |
0.80 |
| Drug onset (Sec) |
159 |
31 |
150 |
32 |
0.23 |
| TOF ratio (pre deep relaxation) |
0.3 |
0.1 |
0.3 |
0.2 |
0.78 |
| TOF count (reverse) |
2.9 |
0.8 |
2.6 |
1.1 |
0.18 |
| Post tetanic count (pre deep relaxation) |
4.9 |
1.4 |
4.4 |
2.3 |
0.26 |
| D1 (cm) |
36.2 |
3.5 |
36.8 |
3.2 |
0.47 |
| D2 (cm) |
40.3 |
4.1 |
41.6 |
3.8 |
0.18 |
| D3 (cm) |
42.9 |
4.0 |
44.0 |
4.3 |
0.25 |
| ∆21 (cm) |
4.1 |
2.1 |
4.8 |
2.3 |
0.19 |
| ∆31 (cm) |
6.6 |
2.3 |
7.2 |
2.8 |
0.37 |
| ∆32 (cm) |
2.6 |
1.3 |
2.4 |
1.3 |
0.62 |
SBP, systolic blood pressure; DBP, Diastolic blood pressure; MAP, Mean arterial pressure; HR, Heart rate.
Figures 2a-2c show the average changes in XPD in different stages of the surgery. The changes in IA group (∆21 = 4.8) were slightly more than in TIVA group (∆21 = 4.1), but this difference was not statistically significant (P = 0.19). This trend is also the case for the mean comparison before and after deep relaxation. The changes in the amount of relaxation in the IA group (∆31 = 7.2) is more than TIVA group (∆31 = 6.6), however the observed difference is not statistically significant (P = 0.37). The changes in ∆32 in TIVA group were slightly more than IA group, but again the difference was not statistically significant (P = 0.62).
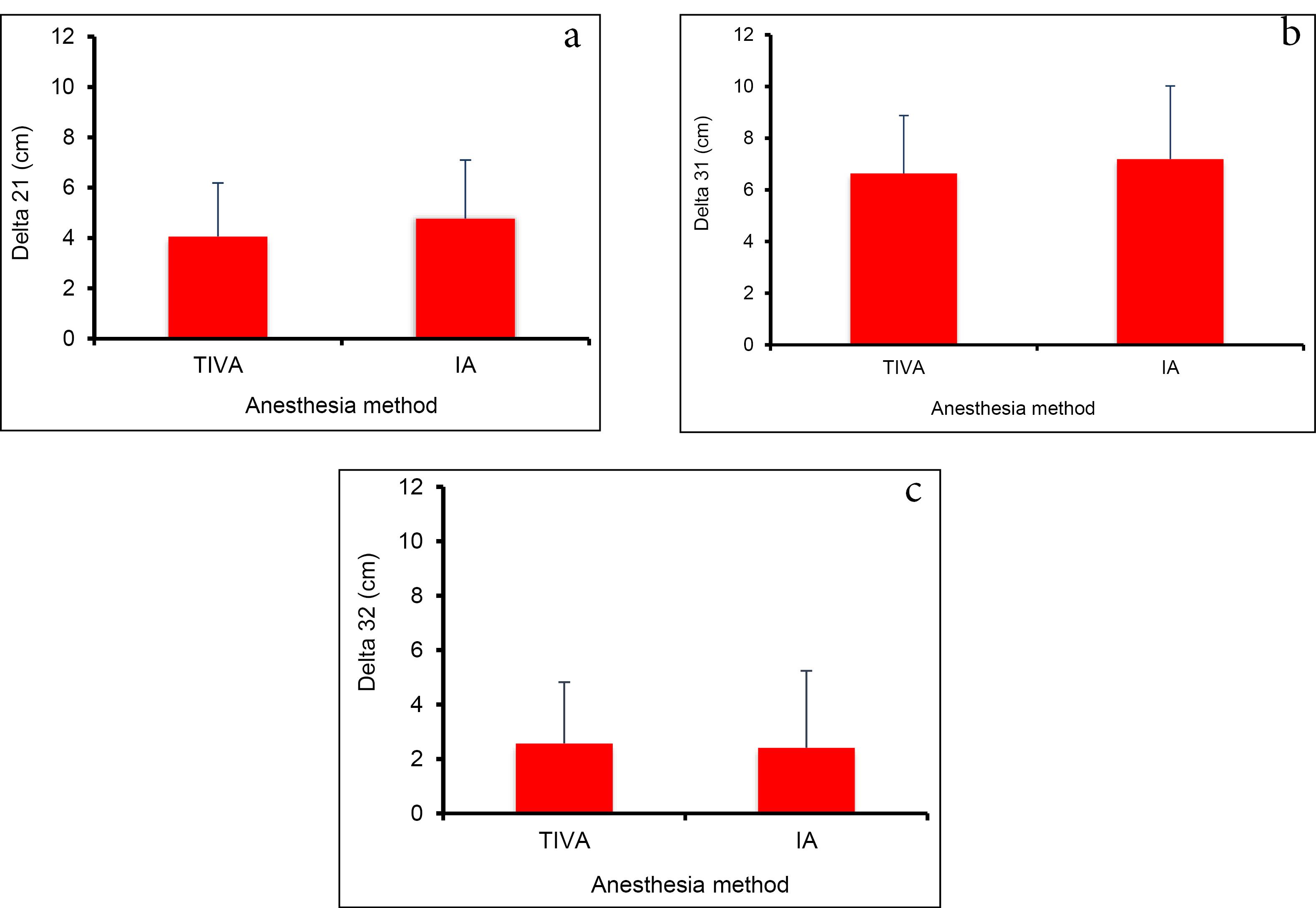
Figure 2.
Average changes in the XPD in different stages of the surgery, (a) distance before induction and after gas insufflation, (b) distance before induction and after deep relaxation, and (c) distance after gas insufflation and deep relaxation. XPD: xiphopubic distance, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
.
Average changes in the XPD in different stages of the surgery, (a) distance before induction and after gas insufflation, (b) distance before induction and after deep relaxation, and (c) distance after gas insufflation and deep relaxation. XPD: xiphopubic distance, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
The comparison of the findings related to the surgical conditions declared by the surgeon’s in TIVA and IA groups is shown in Figure 3. The results of χ2 analysis show that there is no significant difference in the frequencies observed in two groups (P = 0.41). The sums of relative frequencies for optimal and good conditions in TIVA and IA groups are 97% and 91%, which is more than the reported value by Koo et al for deep relaxation group ( = 69%) in LC surgeries. The corresponding value for moderate relaxation was 34%8 according to four point scale. The reported values for laparoscopic hysterectomy in deep relaxation group was 90% and in moderate relaxation group was 66%.20 The relative frequencies for optimal and good conditions for laparoscopic prostatectomy or nephrectomy were 99% and 82%, respectively for deep and moderate relaxation groups.14 Beside the differences in the type and location of the surgeries, the surgeon’s satisfaction in deep relaxation groups was better than moderate relaxation group.

Figure 3.
The frequency of surgeon’s declared satisfaction. TIVA: total intravenous anesthesia, IA: inhalation anesthesia
.
The frequency of surgeon’s declared satisfaction. TIVA: total intravenous anesthesia, IA: inhalation anesthesia
Figure 4 illustrate the hemodynamic changes during deep relaxation in TIVA and IA groups. Comparison of the effect of propofol (TIVA) and isoflurane (IA) on LC revealed that there were lower systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR) and mean arterial pressure (MAP) of post deep relaxation than pre-deep relaxation suggested that both TIVA and IA can stabilize hemodynamics after deep relaxation. An intra-abdominal pressure of 30 to 40 mm Hg does not pose a serious risk of hemodynamic changes.21,22 The results of an experimental study on the mechanism of hemodynamic changes caused by CO2 insufflation at a pressure of 15 mm Hg compared to blowing nitrogen showed that the main hemodynamic changes were caused by the absorption of carbon dioxide and at this pressure the effect of mechanical pressure was not significant.23 The effects of standard (12.16 mm Hg) and low (8.10 mm Hg) pressure insufflation of CO2 on intracranial pressure of patients under LC were investigated and found no significant effect on intracranial pressure.24
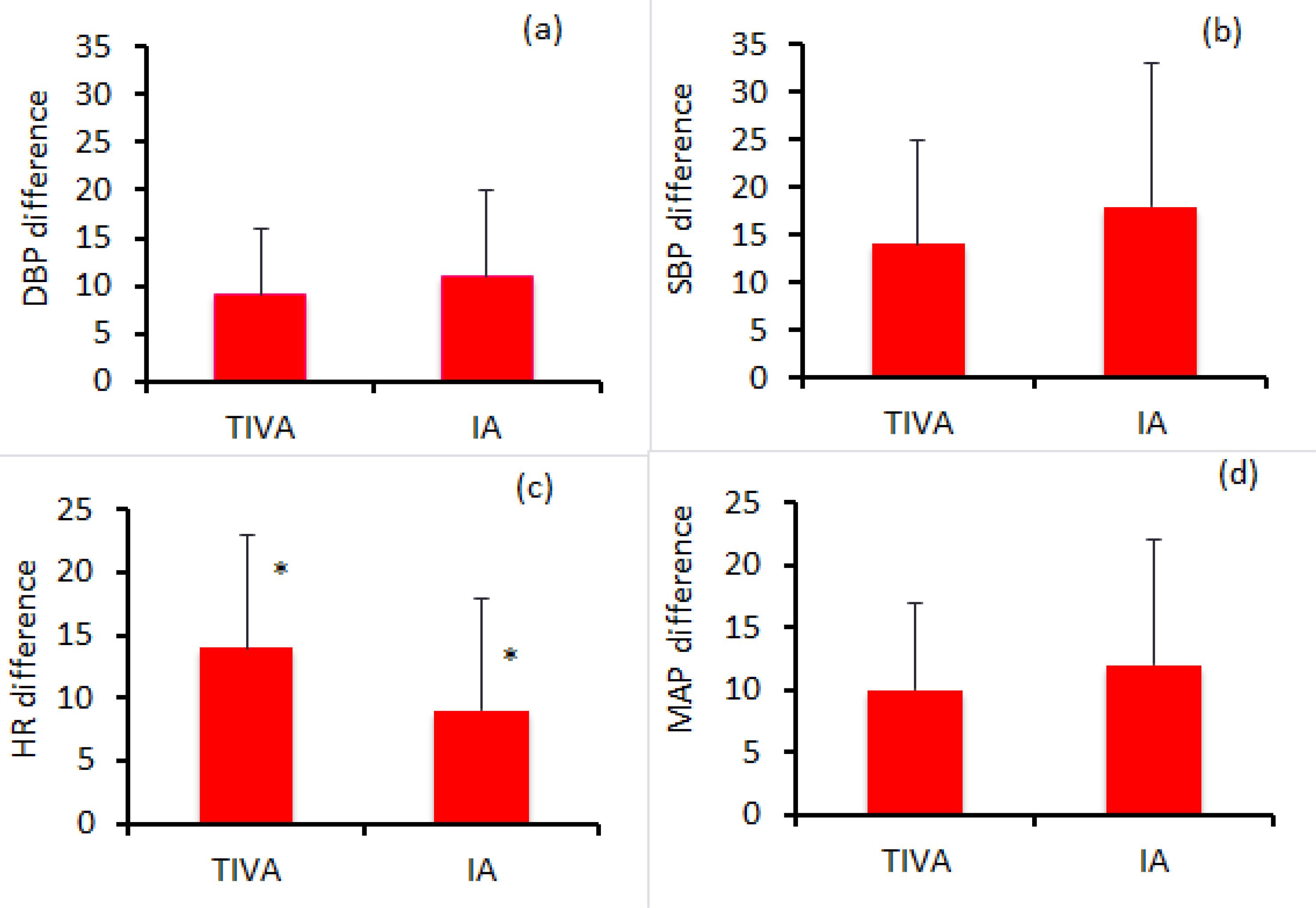
Figure 4.
Average changes in hemodynamic parameters; a: diastolic blood pressure difference, b: systolic blood pressure difference, c: heart rate difference (*: difference was statistically significant), p < 0.05, and d: mean arterial blood pressure difference. TIVA, total intravenous anesthesia; IA, inhalation anesthesia; SBP, systolic blood pressure; DBP, Diastolic blood pressure; MAP, Mean arterial pressure; HR, Heart rate
.
Average changes in hemodynamic parameters; a: diastolic blood pressure difference, b: systolic blood pressure difference, c: heart rate difference (*: difference was statistically significant), p < 0.05, and d: mean arterial blood pressure difference. TIVA, total intravenous anesthesia; IA, inhalation anesthesia; SBP, systolic blood pressure; DBP, Diastolic blood pressure; MAP, Mean arterial pressure; HR, Heart rate
The average drug onset time (Figure 5) in the two studied groups were compared and despite the slightly longer onset time (9 seconds) for TIVA group, the observed difference with IA group was not statistically significant (P = 0.23).
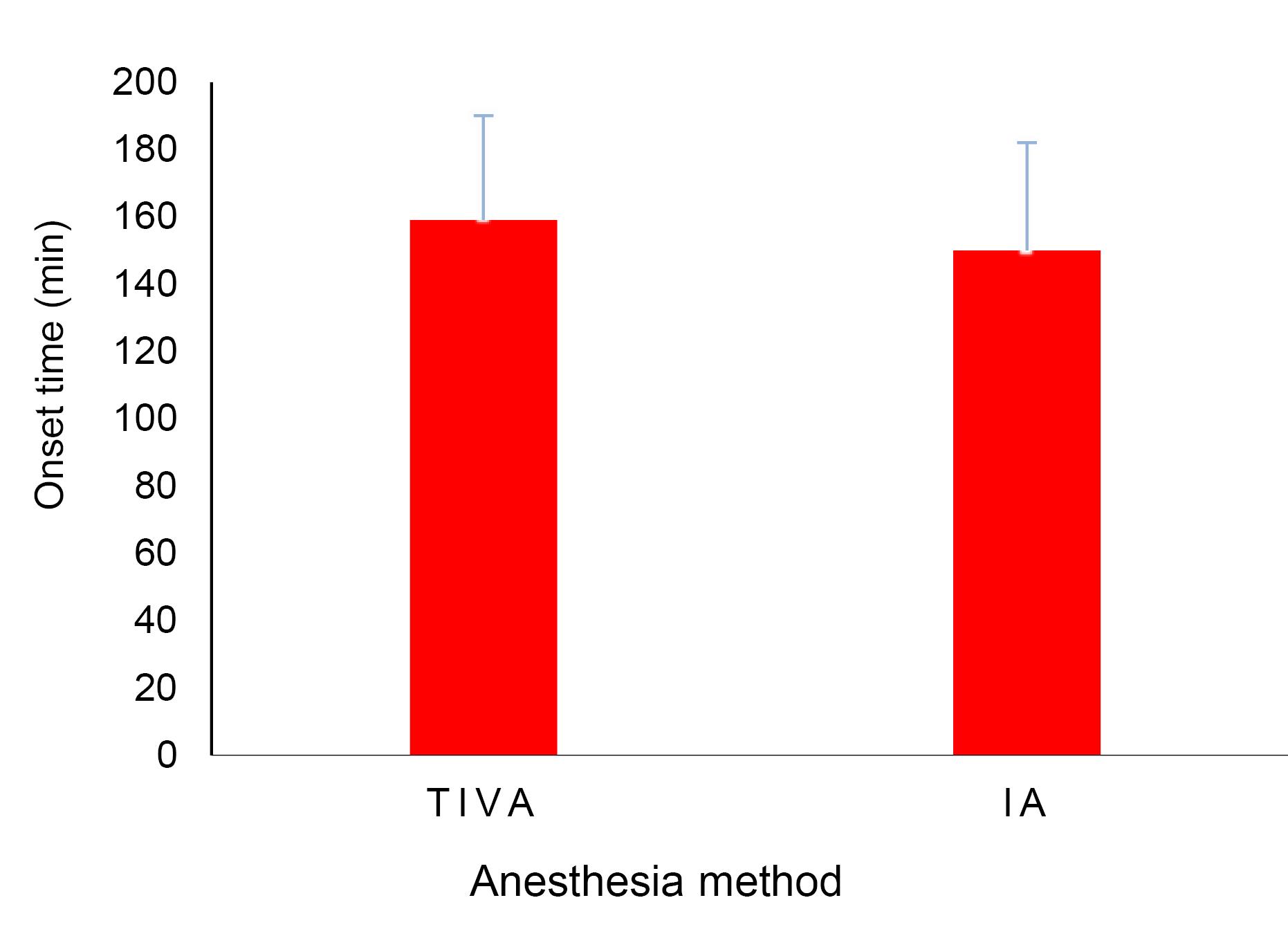
Figure 5.
Drug onset time for TIVA and IA groups, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
.
Drug onset time for TIVA and IA groups, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
Figure 6 compares the TOF ratio for TIVA and IA groups. The relaxation in both groups is equivalent and no significant difference (P = 0.78) was observed.
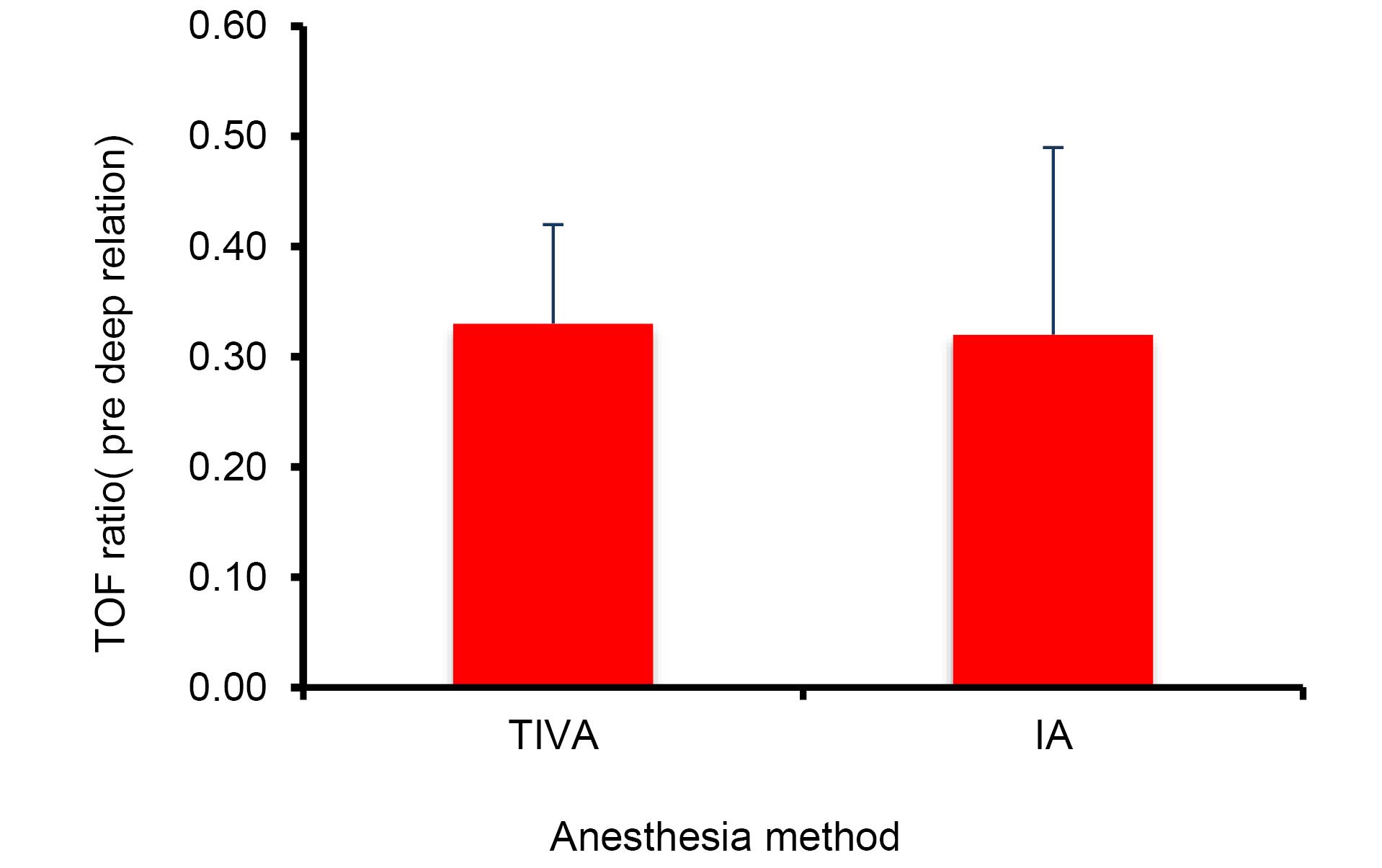
Figure 6.
Train of four ratios before deep relaxation for TIVA and IA groups, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
.
Train of four ratios before deep relaxation for TIVA and IA groups, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
The mean PTC (Figure 7) in TIVA group was slightly more ( = 0.5) than IA group, but this difference was not significant (P = 0.26).
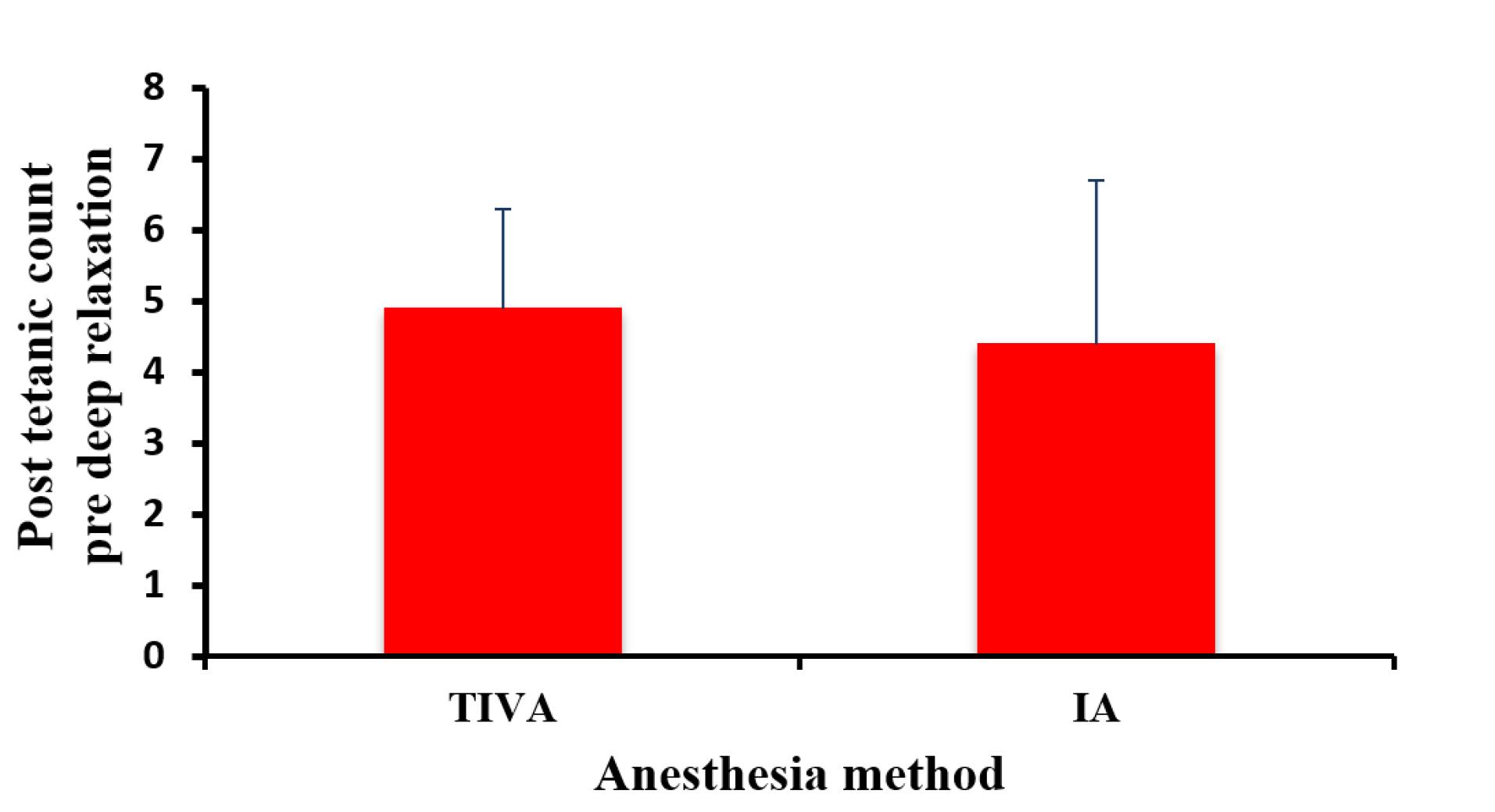
Figure 7.
Post tetanic counts before deep relaxation for TIVA and IA groups, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
.
Post tetanic counts before deep relaxation for TIVA and IA groups, TIVA: total intravenous anesthesia, IA: inhalation anesthesia
The responses of different muscles against the NMBs are not uniform and usually abdominal muscles and diaphragm recover faster than adductor pollicis muscle which is used for monitoring of the relaxation25,26 and the movement of diaphragm is even possible in deep relaxation.27 In our study, in four cases (11.4%) of TIVA group (or 5.7% for all studied patients in this work) which is more than that of 3.1 % for deep relaxation group reported by Koo et al.8
As an overall discussion, each method has certain advantages, and there is no general consensus regarding their priority and there is also a controversy among anesthesiologists.28-31 Duan et al. conducted a meta-analysis on 10 controlled clinical trials and observed that the QoR-40 measure was higher for TIVA than IA.10 This finding is contrary to the findings of Min et al, who did not report a significant difference between the two groups.32 The length of hospital stay of patients also indicated that there was no significant difference between the two anesthesia methods.10 This finding is in agreement with the results of a meta-analysis on the data of hospital stay of non-cardiac surgeries using TIVA and IA methods reported by Miller et al.33
IA intensifies the effects of muscle relaxants, an effect that is less observed for TIVA. Honing et al34 systematically reviewed the effect of deep muscle relaxation on surgical conditions and their relationship with TIVA or IA. They showed that the operating conditions in laparoscopic kidney surgeries in deep and moderate relaxation did not have a significant difference after maintaining anesthesia with sevoflurane and insufflation of carbon dioxide with a pressure of 12 mm Hg, and the satisfaction of the surgeon in most cases have been good or excellent, even in the medium relaxation.34 This finding is contrary to a previous report of Staehr-Rye et al35 which evaluated the effect of deep relaxation caused by rocuronium (bolus + maintenance infusion with PTC of 0-1 and moderate relaxation (bolus injection of rocuronium and repetition if needed) on 48 patients undergoing elective LC. After receiving propofol, remifentanil and rocuronium, the patients were randomly divided into two groups of deep relaxation (n = 25) and moderate relaxation (n = 23). Surgery with a pressure of 8 mm Hg was started and increased to 12 mm Hg or more if necessary. In the deep relaxation group, surgery was performed on 15 patients with a pressure of 8 mm Hg, and in 10 patients, increased pressure was used to meet the surgical conditions. The numbers in the moderate relaxation group were 8 and 15 patients, respectively. The overall results indicated that the proportion of optimal surgical conditions in the deep relaxation group was somewhat more than that of the moderate relaxation group.35
According to Bruintjes et al,3 deep relaxation at both standard pressure (12 mm Hg) and low pressure (8 mm Hg) increased the intra-abdominal space. Another study that compared the combination of deep relaxation + low pressure and moderate relaxation + standard pressure showed a reduction in shoulder pain after surgery in the deep relaxation + low pressure group without increasing the duration of surgery. In three other studies, in patients with deep and moderate relaxation, surgery was started with low pressure and if the working space was insufficient, the pressure was increased. The results of these three studies showed that the need to increase the pressure in deep relaxation was less. Finally, in a study that measured the minimum pressure necessary to create a suitable working environment, the average pressure was significantly lower in the group with deep than moderate relaxation.3 Barrio et al36 studied the effect of relaxation depth on surgical conditions in low IAP on 90 patients undergoing LC. Patients in three groups, (1) low IAP (8 mm Hg) with moderate relaxation during surgery, (2) low IAP (8 mm Hg) with deep relaxation during surgery and 3) standard IAP (12 mm Hg). Group 1 patients received rocuronium infusion (at a concentration of 1 mg/mL) and titrated to achieve a TOF of 1-3, group 2 patients received an additional bolus dose of 0.6 mg/kg following rocuronium infusion and a PTC of 1-5. This group received sugammadex (with a dose of 2 mg/kg for group 1 and 4 mg/kg for group 2) and relaxation monitoring was continued until the TOF ratio of > 90%. In group 3 patients, who were considered as the control group, the standard clinical method of the hospital was used for preoperative preparation. Anesthesia induction and maintenance were performed according to the anesthesiologist’s opinion, and relaxant drugs were used. The use of neuromuscular block and maintenance of anesthesia by propofol infusion and titration with bispectral index of 40-60 were at the disposal of the anesthesiologist.37 The results of the study showed that in terms of good surgical conditions (level I: optimal conditions and level II: sufficient conditions for surgery) and bad (level III: acceptable conditions), an intervention was considered to improve surgical conditions, and level IV: poor conditions, surgery was not acceptable and intervention was necessary to continue the surgery) in groups 1 and 2, there was no significant difference in terms of surgical conditions and duration of surgery. When the conditions of level I surgery were compared in two groups, despite the fact that the frequency of level I conditions in group 2 (deep relaxation) was more than that of group 1, but the difference in frequency between the two groups was not statistically significant. The most important finding of this study was the lack of determining effect of the relaxation depth on the improvement of surgical conditions and performing surgery in low IAP by experienced surgeons. On the other hand, better surgical conditions were observed in standard IAP regardless of the depth of relaxation.36 Koo and colleagues8 studied the effects of deep relaxation and low IAP in LC surgeries and concluded that the use of deep relaxation reduces the need to increase IAP. In this study, 64 patients were studied in the deep relaxation (PTC of 1 or 2) and moderate relaxation (TOF of 1 or 2) groups. Relaxation was induced in both groups with rocuronium and reversed by sugammadex in the deep relaxation group and with neostigmine in the moderate relaxation group. At the beginning of the surgery, the IAP was set at 8 mm Hg and the condition was checked by the surgeon and the pressure was increased if necessary. The frequency of the cases in which the IAP increased during surgery was 12.5% and 34.4% for the deep and moderate relaxation groups, respectively, and this frequency difference was statistically significant.8
Most of the studies conducted on the benefits of deep relaxation have been performed in patients undergoing low-risk intra-abdominal surgeries or bariatric surgeries.14,34,38-46 Today, neuromuscular block is commonly used in abdominal surgeries, but the routine use of deep relaxation is still controversial. A systematic review presented by Madsen et al47 showed the improvement of surgical conditions following the use of deep relaxation, while another systematic review Kopman and Naguib in the same year (i.e. 2016) showed the lack of sufficient evidence for the use of deep relaxation in laparoscopic surgeries, and there is no evidence of superiority of moderate over deep relaxation.48
Conclusion
Abdominal surgery is increasingly performed by laparoscopy. To improve the surgeon’s working conditions in laparoscopic procedures, the interest in the potential beneficial effects of deep muscle block to prevent patient movements and abdominal contractions has greatly increased and improved surgical outcomes such as reducing mortality, complications or accidents during surgery.
This study examined the effects of rocuronium -induced deep relaxation with two methods of IA and TIVA on the conditions and quality of surgery, the abdominal compliance and the recovery profile. The comparison of the abdominal compliance with a constant pressure of CO2 insufflation in LC surgery is shown in both methods of anesthesia. The findings showed that deep relaxation causes a greater increase in abdominal distention and an increase in the XPD and allows the surgeon for better performance. These effects were not significantly different in IA and TIVA groups. Deep relaxation decisively improves the conditions of surgery and provides complete satisfaction of the surgeon, and there is no significant difference of surgeon’s satisfaction and the operation conditions with deep relaxation between the two methods of anesthesia.
The effect of deep relaxation on the XPD was measured as a reflection of the increase in the abdomen volume. There is a relationship between XPD, as a feasible and simple measure of abdominal laxity, and the surgeon’s satisfaction, and it shows that the more the abdominal compliance increases, the more the surgeon’s satisfaction, and this could be achieved either by high-pressure gas insufflation or deep relaxation. In high-risk patients, where increased IAP may cause hemodynamic and respiratory complications, deep relaxation can be an alternative method to provide suitable conditions for surgery, prevents sudden muscle contractions during surgery and reduces possible complications.
According to the findings of this research, no significant difference was observed in the investigated interoperative parameters among TIVA and IA methods. Although TIVA has advantages for some patients, IA is still the most commonly used anesthesia method in many operation rooms. There is no overall agreement on superiority of TIVA or IA, both methods are safe and effective and their selection depends on anesthesiologists preference, type of surgery, patients conditions and availability of monitoring systems. The proposed procedure provides a deep relaxation without a need for costly drug, i.e. sugammadex, as a reversing agent and is more suitable for low income communities.
Competing Interests
There is no conflict of interest.
Consent for Publication
Written informed consent for publication has been obtained from the participants in this study.
Data Availability Statement
All data generated or analysed during this study are included in this published article.
Ethical Approval
All steps and goals of the project were completely explained to the patients participating in this project and they signed an informed consent form approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1401.141). The executive protocol of this study has been registered in the National Clinical Trials Registration System and has received IRCT20220519054914N1 license code.
Acknowledgements
This report is a part of the results of M. Khoubnasabjafari thesis submitted to the Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran. The authors would like to thank surgeons and technical staff for their valuable contribution in this work.
References
- Aerts R, Penninckx F. The burden of gallstone disease in Europe. Aliment Pharmacol Ther 2003; 18 Suppl 3:49-53. doi: 10.1046/j.0953-0673.2003.01721.x [Crossref] [ Google Scholar]
- Barkun JS, Barkun AN, Meakins JL. Laparoscopic versus open cholecystectomy: the Canadian experience The McGill Gallstone Treatment Group. Am J Surg 1993; 165(4):455-8. doi: 10.1016/s0002-9610(05)80940-7 [Crossref] [ Google Scholar]
- Bruintjes MH, van Helden EV, Braat AE, Dahan A, Scheffer GJ, van Laarhoven CJ. Deep neuromuscular block to optimize surgical space conditions during laparoscopic surgery: a systematic review and meta-analysis. Br J Anaesth 2017; 118(6):834-42. doi: 10.1093/bja/aex116 [Crossref] [ Google Scholar]
- Umar A, Mehta KS, Mehta N. Evaluation of hemodynamic changes using different intra-abdominal pressures for laparoscopic cholecystectomy. Indian J Surg 2013; 75(4):284-9. doi: 10.1007/s12262-012-0484-x [Crossref] [ Google Scholar]
- Amin AM, Mohammad MY, Ibrahim MF. Comparative study of neuromuscular blocking and hemodynamic effects of rocuronium and cisatracurium under sevoflurane or total intravenous anesthesia. Middle East J Anaesthesiol 2009; 20(1):39-51. [ Google Scholar]
- Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006(4):CD006231. doi: 10.1002/14651858.Cd006231.
- Fuchs-Buder T, Meistelman C, Raft J. Sugammadex: clinical development and practical use. Korean J Anesthesiol 2013; 65(6):495-500. doi: 10.4097/kjae.2013.65.6.495 [Crossref] [ Google Scholar]
- Koo BW, Oh AY, Seo KS, Han JW, Han HS, Yoon YS. Randomized clinical trial of moderate versus deep neuromuscular block for low-pressure pneumoperitoneum during laparoscopic cholecystectomy. World J Surg 2016; 40(12):2898-903. doi: 10.1007/s00268-016-3633-8 [Crossref] [ Google Scholar]
- Madsen MV, Staehr-Rye AK, Claudius C, Gätke MR. Is deep neuromuscular blockade beneficial in laparoscopic surgery? Yes, probably. Acta Anaesthesiol Scand 2016; 60(6):710-6. doi: 10.1111/aas.12698 [Crossref] [ Google Scholar]
- Duan RR, Zhang Q, Qin XY, Wang CA. Effect of total intravenous anesthesia and inhalation anesthesia on recovery quality of patients after laparoscopic surgery: a systematic review and meta-analysis. Asian J Surg 2023; 46(8):3234-5. doi: 10.1016/j.asjsur.2023.03.008 [Crossref] [ Google Scholar]
- Parab S, Gaikwad S, Majeti S. Inhalational versus intravenous anesthetics during one lung ventilation in elective thoracic surgeries: a narrative review. Saudi J Anaesth 2021; 15(3):312-23. doi: 10.4103/sja.sja_1106_20 [Crossref] [ Google Scholar]
- Baskaran A, Arun Kumar A, Vijayakumar D, Balamurugan B. Comparison of efficacy of atracurium versus cisatracurium in patients undergoing surgeries under general anasethesia. Ann Trop Med Public Health 2020; 23(S14):SP231519. doi: 10.36295/asro.2020.231519 [Crossref] [ Google Scholar]
- Greenberg SB, Vender J. The use of neuromuscular blocking agents in the ICU: where are we now?. Crit Care Med 2013; 41(5):1332-44. doi: 10.1097/CCM.0b013e31828ce07c [Crossref] [ Google Scholar]
- Martini CH, Boon M, Bevers RF, Aarts LP, Dahan A. Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block. Br J Anaesth 2014; 112(3):498-505. doi: 10.1093/bja/aet377 [Crossref] [ Google Scholar]
- Turhanoğlu S, Tunç M, Okşar M, Temiz M. Perioperative effects of induction with high-dose rocuronium during laparoscopic cholecystectomy. Turk J Anaesthesiol Reanim 2020; 48(3):188-95. doi: 10.5152/tjar.2019.31855 [Crossref] [ Google Scholar]
- Critchley LA, Critchley JA, Gin T. Haemodynamic changes in patients undergoing laparoscopic cholecystectomy: measurement by transthoracic electrical bioimpedance. Br J Anaesth 1993; 70(6):681-3. doi: 10.1093/bja/70.6.681 [Crossref] [ Google Scholar]
- Gehring H, Kuhmann K, Klotz KF, Ocklitz E, Roth-Isigkeit A, Sedemund-Adib B. Effects of propofol vs isoflurane on respiratory gas exchange during laparoscopic cholecystectomy. Acta Anaesthesiol Scand 1998; 42(2):189-94. doi: 10.1111/j.1399-6576.1998.tb05107.x [Crossref] [ Google Scholar]
- Tan PL, Lee TL, Tweed WA. Carbon dioxide absorption and gas exchange during pelvic laparoscopy. Can J Anaesth 1992; 39(7):677-81. doi: 10.1007/bf03008229 [Crossref] [ Google Scholar]
- Blobner M, Felber AR, Gögler S, Weigl EM, Esselborn SJ. Carbon dioxide uptake from pneumoperitoneum during laparoscopic cholecystectomy. Anesthesiology 1992; 77(3A Suppl):A37. [ Google Scholar]
- Dubois PE, Putz L, Jamart J, Marotta ML, Gourdin M, Donnez O. Deep neuromuscular block improves surgical conditions during laparoscopic hysterectomy: a randomised controlled trial. Eur J Anaesthesiol 2014; 31(8):430-6. doi: 10.1097/eja.0000000000000094 [Crossref] [ Google Scholar]
- Kashtan J, Green JF, Parsons EQ, Holcroft JW. Hemodynamic effects of increased abdominal pressure. J Surg Res 1981; 30(3):249-55. doi: 10.1016/0022-4804(81)90156-6 [Crossref] [ Google Scholar]
- Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intraabdominal pressure. J Surg Res 1987; 43(1):14-20. doi: 10.1016/0022-4804(87)90041-2 [Crossref] [ Google Scholar]
- Ho HS, Saunders CJ, Gunther RA, Wolfe BM. Effector of hemodynamics during laparoscopy: CO2 absorption or intra-abdominal pressure?. J Surg Res 1995; 59(4):497-503. doi: 10.1006/jsre.1995.1198 [Crossref] [ Google Scholar]
- Saini V, Samra T, Sethi S, Naik BN. Comparative evaluation of optic nerve sheath diameter in patients undergoing laparoscopic cholecystectomy using low and standard pressures of gas insufflations. J Anaesthesiol Clin Pharmacol 2021; 37(4):616-21. doi: 10.4103/joacp.JOACP_370_18 [Crossref] [ Google Scholar]
- Kirov K, Motamed C, Dhonneur G. Differential sensitivity of abdominal muscles and the diaphragm to mivacurium: an electromyographic study. Anesthesiology 2001; 95(6):1323-8. doi: 10.1097/00000542-200112000-00008 [Crossref] [ Google Scholar]
- Donati F, Meistelman C, Plaud B. Vecuronium neuromuscular blockade at the adductor muscles of the larynx and adductor pollicis. Anesthesiology 1991; 74(5):833-7. doi: 10.1097/00000542-199105000-00006 [Crossref] [ Google Scholar]
- Fernando PU, Viby-Mogensen J, Bonsu AK, Tamilarasan A, Muchhal KK, Lambourne A. Relationship between posttetanic count and response to carinal stimulation during vecuronium-induced neuromuscular blockade. Acta Anaesthesiol Scand 1987; 31(7):593-6. doi: 10.1111/j.1399-6576.1987.tb02627.x [Crossref] [ Google Scholar]
- Kolia NR, Man LX. Total intravenous anaesthesia versus inhaled anaesthesia for endoscopic sinus surgery: a meta-analysis of randomized controlled trials. Rhinology 2019; 57(6):402-10. doi: 10.4193/Rhin19.171 [Crossref] [ Google Scholar]
- Kim SH, Ju HM, Choi CH, Park HR, Shin S. Inhalational versus intravenous maintenance of anesthesia for quality of recovery in patients undergoing corrective lower limb osteotomy: a randomized controlled trial. PLoS One 2021; 16(2):e0247089. doi: 10.1371/journal.pone.0247089 [Crossref] [ Google Scholar]
- Liu T, Gu Y, Chen K, Shen X. Quality of recovery in patients undergoing endoscopic sinus surgery after general anesthesia: total intravenous anesthesia vs desflurane anesthesia. Int Forum Allergy Rhinol 2019; 9(3):248-54. doi: 10.1002/alr.22246 [Crossref] [ Google Scholar]
- de Carli D, Meletti JF, Neto NE, Martinez G, Kim AL, de Camargo RP. General anesthesia technique and perception of quality of postoperative recovery in women undergoing cholecystectomy: a randomized, double-blinded clinical trial. PLoS One 2020; 15(2):e0228805. doi: 10.1371/journal.pone.0228805 [Crossref] [ Google Scholar]
- Shui M, Xue Z, Miao X, Wei C, Wu A. Intravenous versus inhalational maintenance of anesthesia for quality of recovery in adult patients undergoing non-cardiac surgery: a systematic review with meta-analysis and trial sequential analysis. PLoS One 2021; 16(7):e0254271. doi: 10.1371/journal.pone.0254271 [Crossref] [ Google Scholar]
- Miller D, Lewis SR, Pritchard MW, Schofield-Robinson OJ, Shelton CL, Alderson P. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst Rev 2018; 8(8):CD012317. doi: 10.1002/14651858.CD012317.pub2 [Crossref] [ Google Scholar]
- Honing GH, Martini CH, Olofsen E, Bevers RF, Huurman VA, Alwayn IP. Deep neuromuscular block does not improve surgical conditions in patients receiving sevoflurane anaesthesia for laparoscopic renal surgery. Br J Anesth 2021; 126(2):377-85. doi: 10.1016/j.bja.2020.09.024 [Crossref] [ Google Scholar]
- Staehr-Rye AK, Rasmussen LS, Rosenberg J, Juul P, Lindekaer AL, Riber C. Surgical space conditions during low-pressure laparoscopic cholecystectomy with deep versus moderate neuromuscular blockade: a randomized clinical study. Anesth Analg 2014; 119(5):1084-92. doi: 10.1213/ane.0000000000000316 [Crossref] [ Google Scholar]
- Barrio J, Errando CL, García-Ramón J, Sellés R, San Miguel G, Gallego J. Influence of depth of neuromuscular blockade on surgical conditions during low-pressure pneumoperitoneum laparoscopic cholecystectomy: a randomized blinded study. J Clin Anesth 2017; 42:26-30. doi: 10.1016/j.jclinane.2017.08.005 [Crossref] [ Google Scholar]
- Colin P, Eleveld DJ, van den Berg JP, Vereecke HE, Struys M, Schelling G. Propofol breath monitoring as a potential tool to improve the prediction of intraoperative plasma concentrations. Clin Pharmacokinet 2016; 55(7):849-59. doi: 10.1007/s40262-015-0358-z [Crossref] [ Google Scholar]
- van Wijk RM, Watts RW, Ledowski T, Trochsler M, Moran JL, Arenas GW. Deep neuromuscular block reduces intra-abdominal pressure requirements during laparoscopic cholecystectomy: a prospective observational study. Acta Anaesthesiol Scand 2015; 59(4):434-40. doi: 10.1111/aas.12491 [Crossref] [ Google Scholar]
- Blobner M, Frick CG, Stäuble RB, Feussner H, Schaller SJ, Unterbuchner C. Neuromuscular blockade improves surgical conditions (NISCO). Surg Endosc 2015; 29(3):627-36. doi: 10.1007/s00464-014-3711-7 [Crossref] [ Google Scholar]
- Rosenberg J, Herring WJ, Blobner M, Mulier JP, Rahe-Meyer N, Woo T. Deep neuromuscular blockade improves laparoscopic surgical conditions: a randomized, controlled study. Adv Ther 2017; 34(4):925-36. doi: 10.1007/s12325-017-0495-x [Crossref] [ Google Scholar]
- Torensma B, Martini CH, Boon M, Olofsen E, In’t Veld B, Liem RS. Deep neuromuscular block improves surgical conditions during bariatric surgery and reduces postoperative pain: a randomized double-blind controlled trial. PLoS One 2016; 11(12):e0167907. doi: 10.1371/journal.pone.0167907 [Crossref] [ Google Scholar]
- Baete S, Vercruysse G, Vander Laenen M, De Vooght P, Van Melkebeek J, Dylst D. The effect of deep versus moderate neuromuscular block on surgical conditions and postoperative respiratory function in bariatric laparoscopic surgery: a randomized, double blind clinical trial. Anesth Analg 2017; 124(5):1469-75. doi: 10.1213/ane.0000000000001801 [Crossref] [ Google Scholar]
- Hu G, Shao W, Chen Z, Li B, Xu B. Deep neuromuscular block attenuates intra-abdominal pressure and inflammation and improves post-operative cognition in prostate cancer patients following robotic-assisted radical prostatectomy. Int J Med Robot 2024; 20:e2565. doi: 10.1002/rcs.2565 [Crossref] [ Google Scholar]
- Yi IK, Kim JS, Hur H, Han DG, Kim JE. Effects of deep neuromuscular block on surgical pleth index-guided remifentanil administration in laparoscopic herniorrhaphy: a prospective randomized trial. Sci Rep 2022; 12(1):19176. doi: 10.1038/s41598-022-23876-5 [Crossref] [ Google Scholar]
- Park SH, Huh H, Choi SI, Kim JH, Jang YJ, Park JM. Impact of the deep neuromuscular block on oncologic quality of laparoscopic surgery in obese gastric cancer patients: a randomized clinical trial. J Am Coll Surg 2022; 234(3):326-39. doi: 10.1097/xcs.0000000000000061 [Crossref] [ Google Scholar]
- Aceto P, Perilli V, Modesti C, Sacco T, De Cicco R, Ceaichisciuc I. Effects of deep neuromuscular block on surgical workspace conditions in laparoscopic bariatric surgery: a systematic review and meta-analysis of randomized controlled trials. Minerva Anestesiol 2020; 86(9):957-64. doi: 10.23736/s0375-9393.20.14283-4 [Crossref] [ Google Scholar]
- Madsen MV, Staehr-Rye AK, Gätke MR, Claudius C. Neuromuscular blockade for optimising surgical conditions during abdominal and gynaecological surgery: a systematic review. Acta Anaesthesiol Scand 2015; 59(1):1-16. doi: 10.1111/aas.12419 [Crossref] [ Google Scholar]
- Kopman AF, Naguib M. Is deep neuromuscular block beneficial in laparoscopic surgery? No, probably not. Acta Anaesthesiol Scand 2016; 60(6):717-22. doi: 10.1111/aas.12699 [Crossref] [ Google Scholar]